Data driven transformation
We have developed value-driven solutions in data and analytics, pharmacy, medical, and consumer engagement specifically designed to improve patient care and lower costs. Our solutions harness one-of-a-kind, aggregated cross-carrier and cross-provider data to shape efficient, effective, high-quality healthcare for employees:
- Data and Analytics—aggregating and analyzing data to objectively identify the most effective providers and treatments.
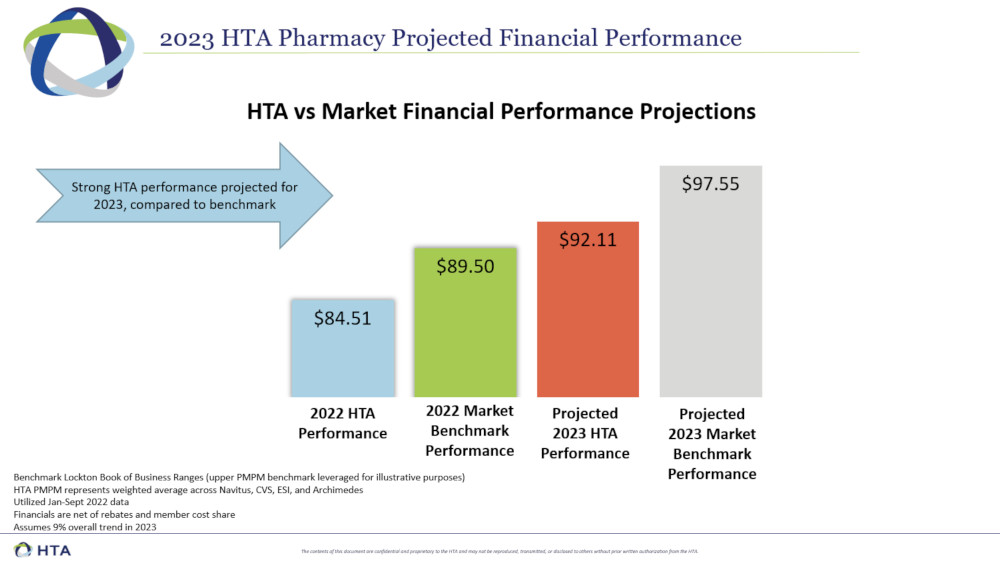
- Pharmacy—member-only Pharmacy Benefit Manager (PBM) partnerships include market-leading terms, increased savings, and formulary development participation —all rooted in financial transparency.
- Consumer Engagement—Consumer technology puts insights into employees’ hands, allowing them to make informed healthcare choices. HTA connects consumers with high value solutions.
- Medical—We help our members flatten their medical cost trend while improving health outcomes and employee benefits affordability. HTA programs help employers reduce waste and inefficiency, improve clinical programs and prevention, and make better care more accessible and affordable.
HTA Members who Carve Out Specialty Drugs from PBM Arrangement Reduce Specialty Spend ~47%
| HTA Member Companies w/no Specialty Carve Out | HTA Member Companies with Specialty Carve Out | |
|---|---|---|
| Non-Specialty Plan Cost PMPM | $30.74 | $22.77 |
| Specialty Plan Cost PMPM | $58.07 | $30.66 |
| Total Plan Cost PMPM | $88.81 | $53.43 |
Actionable insight
We aggregate data across more than three million covered lives. Our unique and proprietary dataset provides dynamic cross-geography insights, including:
Provider-level analytics
Insights across all types of spend
Anonymized claims from multiple sources